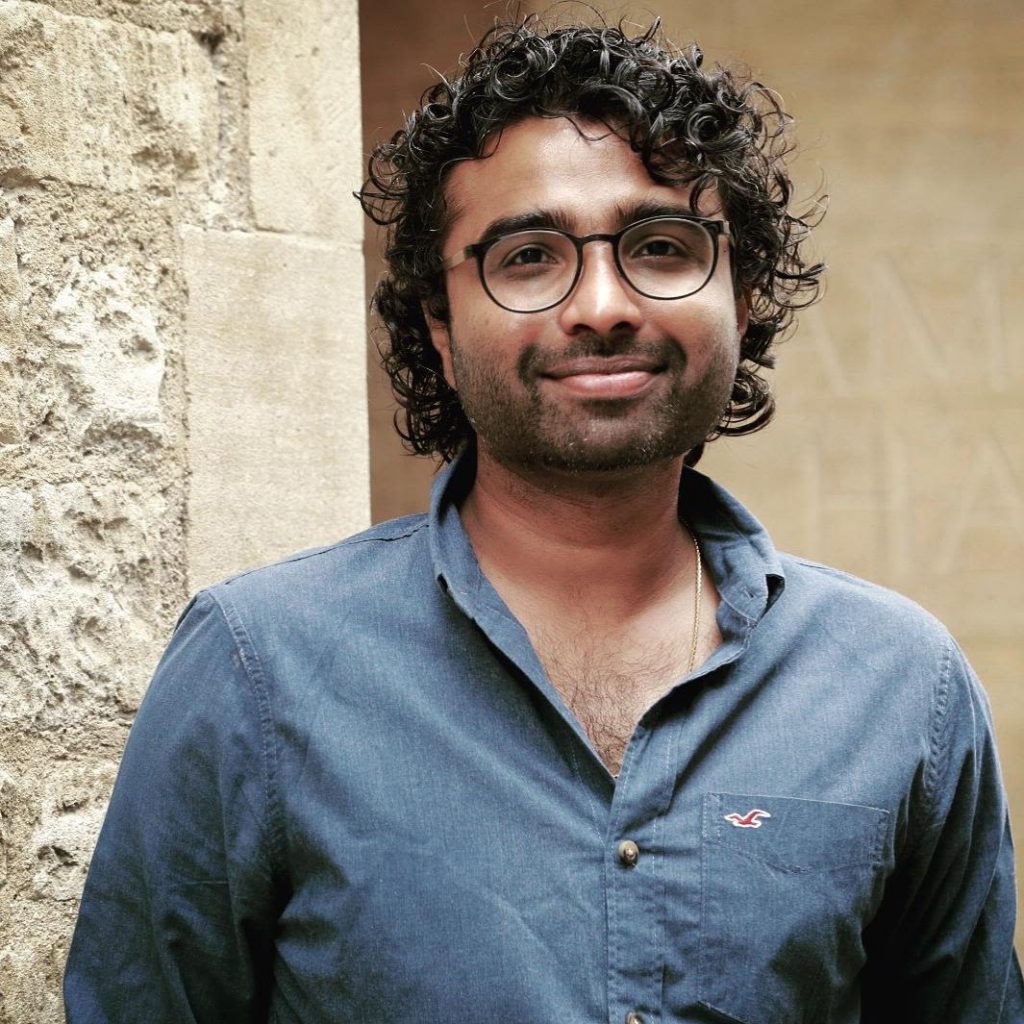
Arun Joseph, a DPhil student in Clinical Neurosciences, is a qualified physiotherapist, specialising in critical care and respiratory physiotherapy. He tells us about his journey to Oxford and the research he’s doing to enable better outcomes for critically-ill patients requiring ventilation while in intensive care.
I’m from Kanniyakumari (Cape Comorin), which is the southernmost tip of India. It is also the culmination point of the Arabian Sea, the Bay of Bengal and the Indian Ocean. I completed an undergraduate programme in physiotherapy in India, and started working within critical care from very early on. I moved to Glasgow to pursue a postgraduate research programme in physiotherapy before embarking on a career in the NHS as a critical care and respiratory physiotherapist. I have worked in a variety of settings, including respiratory medicine, surgery, cardiac rehabilitation, general and specialist intensive care units, and always enjoyed on-call emergency adult and paediatric respiratory physiotherapy.
I wanted myself and my research to thrive in a culturally-rich diverse college
I’m currently a first year DPhil student at Jesus College, and have completed 4 months so far. I was born on March 1st – St. David’s Day – so couldn’t chose a better college for my calling! That aside, Jesus is such a friendly inclusive community, and I wanted myself and my research to thrive in a culturally-rich diverse college where every step of mine will be supported and well cared for. I am involved in the college choir, meet the college Chaplain once a month and try to participate in as many events as I can.
The field is lacking clear scientific evidence on how we can get patients safely off the ventilators
Critical care physiotherapists play an important role, not only in rehabilitation, but also in ventilator weaning and extubation in intensive care units. Weaning is the process of gradually reducing a seriously-ill patient’s ventilator support, and extubation is the process of removal of the airway that connects the patient’s lungs to the ventilator. If we leave patients on a ventilator for longer than needed, or disconnect prematurely, it can lead to complications such as ventilator-associated pneumonia, increased ventilator days and increased morbidity and mortality. The failure rates, especially in neurocritical care, are higher than in general adult Intensive Care Units. Currently the field is lacking clear scientific evidence on how we can get patients safely off the ventilators.
Arun and his colleagues in the Respiratory Physiology and Biomedical Engineering Group at the Nuffield Department of Clinical Neurosciences.
I felt that it was crucial to find a way to make the correct clinical judgement on when and how we safely get patients off the ventilator. The problem is multifactorial and so high-quality, interdisciplinary clinical research is the only way forward. My research focusses on two main elements to address this challenge:
- What is the pathophysiology – or the functional changes that occur in the body – of failed extubations in neurocritical care patients? This information helps us to understand the connection between the brain and the airway, and why these patients fail or are unable to cope when we remove ventilation.
- Once we have established the pathophysiology, we can then develop targeted assessment and treatment approaches to prevent avoidable re-intubations (getting back to ventilators again) and failed extubations, which can increase the incidence of hospital-acquired infections and can be associated with poor outcomes.
There is a clear demand for research of this kind. I conducted an informal clinical expert consultation by contacting multi-professional teams in all the neurocritical care units within UK and it has been reassuring to hear from all the clinicians that this area is in need of quality research and is also an important clinical priority to address. I am supervised by Prof. Andrew Farmery, anaesthetist and Head of Nuffield Department of Anaesthesia and Prof. Louise Rose from King’s College London, who is Research Director for the Provincial Centre of Weaning Excellence at the Michal Garron Hospital, Toronto, Canada
I do love teaching and it is great to integrate what I learn in my DPhil to our physiotherapy students.
However, this research is only part of my working week. I am also a part-time lecturer at Coventry University, teaching undergraduate and postgraduate physiotherapy students two days a week, and the module leader for evidence based practice. I do love teaching and it is great to integrate what I learn in my DPhil to our physiotherapy students. I really enjoy working at Coventry, and the lecturers/professors are great to work with. I try to do occasional clinical shifts through NHS Professionals as well, when I tick off some of my DPhil/lecturing tasks.
I am using this time to build my network
I am very grateful that the current pandemic has not affected my research too much. Whilst it would be ideal to have some face-to-face contact, there are less distractions so I’m able to focus, and online learning helps to gain knowledge from the comforts of your own home. My DPhil has not reached the stage for data collection yet, so this has not impacted on the course of my study. I am using this time to build my network, refine my research question, have regular online supervision, as well as write literature reviews and papers for publication.
The network I’ve set up is called the Neurocritical Care Weaning and Extubation Network and is supported by the Nuffield Department of Clinical Neurosciences. Although new, it has already gained a profile worldwide and I have received interest for collaborative research with other universities. The main aim of this network is to bring together inter-professional and multidisciplinary teams to work through different stages of ventilator weaning and extubation within neurocritical care. As we know, the causes for failure is multifactorial and we need diverse perspectives on addressing the clinical issue. The network will aim to conduct inter-professional and interdisciplinary evidence-based projects, clinical audits and also host talks/seminars from experts in this field. It is also quite a focused area and I felt a strong need that science and the clinical world should work in parallel and simultaneously for us to make an effective contribution. If anyone is interested, please subscribe by sending an email request to neurowean-subscribe@maillist.ox.ac.uk